Chapter Headings
- Introduction
- Screening in Indigenous Peoples and/or Communities
- Primary Prevention
- Management
- Educating for Equity (E4E) Care Framework
- Social Barriers to Desired Diabetes Outcomes
- Facilitating Outcomes Using a Cultural Approach
- Key Concepts for Application of the E4E Care Framework
- Other Relevant Guidelines
- Related Websites
- Author Disclosures
Key Messages
- Indigenous peoples living in Canada are among the highest-risk populations for diabetes and related complications. Screening for diabetes should be carried out earlier and at more frequent intervals.
- Effective prevention strategies are essential and should be grounded in the specific social, cultural and health service contexts of the community. Prediabetes is an important opportunity to prevent or delay diabetes with healthy behaviour interventions and/or metformin.
- Particular attention is needed for Indigenous women and girls of childbearing age, as the high incidence of hyperglycemia in pregnancy (gestational and type 2) and maternal obesity increases the risk of childhood obesity and diabetes in the next generation. Early identification of diabetes in pregnancy is important, and postpartum screening for diabetes in women with a history of gestational diabetes should be performed along with appropriate follow up.
- Diabetes management targets in Indigenous peoples should be no different from the general population. A focus on building a therapeutic relationship with an Indigenous person with diabetes is important rather than a singular emphasis on achieving management targets. The current poor success at achieving management targets highlights the limitations of health services when they are not relevant to the social and cultural contexts of Indigenous peoples.
- A purposeful process of learning and continuous self-reflection is required by the health-care worker to integrate Indigenous-specific contexts within the clinical approach to diabetes management.
Key Messages About Diabetes for Indigenous Peoples and Their Communities
- Many Indigenous communities have families with high rates and high risk of type 2 diabetes. If you are in a community with high rates of diabetes, see a health-care provider to learn about ways to be tested for and prevent diabetes.
- The causes of diabetes are complex. Learning about the medical, social and cultural contributions to diabetes is key to diabetes prevention. In particular, seek to understand the relationships between the history of colonization and the current high rates of diabetes in Indigenous peoples.
- Ask about community initiatives that promote healthy behaviours, such as diabetes walks, weight-loss groups, fitness classes, community kitchens and gardens, and school-based activities for children and teenagers.
- If you are planning a pregnancy or may get pregnant, get screened for diabetes. If you are pregnant and have diabetes or have been diagnosed with gestational diabetes, visit your health-care providers more often, and find out about exercise, breastfeeding and other support groups for pregnant women and new mothers.
Practical Tips for Health-Care Providers Caring For Indigenous Peoples
- Acknowledge the legacy of colonization and its ongoing adverse effects on Indigenous health. This legacy:
- Maintains socioeconomic disadvantage that limits healthy choices (diet, physical activity, adherence to medication, etc.), increases levels of stress, and decreases capacity for self-care and healthy behaviour change;
- Perpetuates a toxic social environment for the individual, family, and community with pervasive and accumulated psychosocial adversities throughout the life-course;
- Stirs experiences of shame and stigma with a diagnosis of diabetes;
- May recall residential school-like conditions with health-care provider expectations that Indigenous peoples with diabetes will acquire diabetes knowledge and produce “test” results.
- In clinical interactions, recognize, explore and acknowledge:
- Discord within the therapeutic relationship that may arise from heightened apprehension by the Indigenous person with diabetes as well as emotional reaction to prejudice, power and authority asserted by health-care providers;
- Interconnectedness between socioeconomic disadvantage, adverse life experiences and capacity for managing diabetes;
- One's own (i.e. the health-care provider's) concepts of health, diabetes care and assumptions about Indigenous perspectives;
- The Indigenous person's preferences and barriers for re-connecting and integrating cultural resources and traditional approaches to care.
- Engage and connect broadly with the Indigenous community to:
- Implement prevention efforts and screening, with special attention to children and pre-gestational women, as well as the building of culturally safe interprofessional teams, diabetes registries and surveillance systems;
- Foster positive relationships at the individual, family and community levels that advocate for family and community resources for Indigenous peoples;
- Include traditional and cultural leadership to learn about local beliefs, practices and healing resources.
Note: In this document, the terms Aboriginal and Indigenous are generally used interchangeably. Indigenous peoples is the term accepted by the United Nations Declaration on the Rights of Indigenous Peoples, and is in increasing usage today. In the Canadian context, there are 3 Aboriginal groups recognized by the Constitution: First Nations, Inuit and Métis. It is important to recognize that while many Indigenous peoples live in their original land-based communities, which are mostly rural or remote, as many as 50% live in cities and towns, and may or may not choose to self-identify. Furthermore, wherever they live, Indigenous peoples' customs can vary greatly, according to band or group affiliation, religion, education or a variety of other factors.
Introduction
Improving health outcomes for Indigenous peoples with diabetes requires sufficient capacity and quality of health-care resources that are grounded in the person's specific social and cultural needs and contexts. Diabetes within the Indigenous population is complex and socially mediated (1,2). In 1 study, Indigenous peoples with diabetes perceived physicians as having limited awareness of the social factors affecting health (3). In contrast, physicians identified individual and systems barriers to exploring these issues. Elucidating the vital relational and culturally informed aspects of care that might enable the facilitation of improved diabetes outcomes requires focusing on culture as a resource. As connection to a traditional world view and way of life can be protective, it is important for health-care providers to be able to appropriately elicit and support Indigenous peoples with diabetes who may want to (re)engage in cultural practices (4,5).
In order to redress the legacy of residential schools and related colonial policies, and to advance the process of reconciliation in Canada, in 2015 the Truth and Reconciliation Commission (TRC) made 94 calls to action related to many domains of public life, including health (6). Within the calls to action, the TRC outlined a health service role in reconciliation through fostering health-care quality and equity specific to the needs of Indigenous peoples and communities. In order to realize that role, the TRC identified that health-care providers must understand how colonization has resulted in the current health status of Indigenous peoples. TRC call number 18 emphasizes that health systems be responsive and mobilize resources to address the distinct needs of Indigenous peoples, calling upon:
“…federal, provincial, territorial, and Aboriginal governments to acknowledge that the current state of Aboriginal health in Canada is a direct result of previous Canadian government policies, including residential schools, and to recognize and implement the health-care rights of Aboriginal people as identified in international law, constitutional law, and under the Treaties” (6).
Indigenous peoples around the globe are disproportionately affected by diabetes (7,8) and related complications. In Canada, age-standardized prevalence rates for diabetes are 17.2% among First Nations individuals living on-reserve, 10.3% among First Nations individuals living off-reserve, and 7.3% among Métis people, compared to 5.0% in the general population (9). A recent study in Alberta suggested that the lifetime risk of diabetes was 8 in 10 for First Nations persons over the age of 18 years compared with 5 in 10 for non-First Nations people (10). Among the Inuit people, the age-standardized prevalence rate of diabetes is comparable to that seen in the general Canadian population, but there is concern that rates will rise with large-scale changes impacting healthy behaviour in the far North (11).
Indigenous individuals are diagnosed at an increasingly younger age (12), have greater severity at diagnosis, develop higher rates of complications (13–15), and experience poorer treatment outcomes. The rising incidence among youth and young adults (12,16,17) has been shown to be accompanied by 2.6 times higher rates of end-stage renal disease (ESRD) and death in First Nations compared to non-First Nations persons diagnosed under 20 years of age (18). Higher prevalence rates of microvascular disease, including chronic kidney disease (CKD) (19), lower limb amputation (20,21), foot abnormalities (22,23), and more severe retinopathy (24) have been found. Indigenous peoples are also burdened by higher rates of cardiovascular disease (CVD) (20,25) and exhibit higher rates of cardiometabolic risk factors, including smoking, obesity and hypertension (19,20,26).
In contrast to the general population, a disproportionate burden of diabetes affects First Nations women (27,28), and may be related to an increased prevalence of diabetes complicating pregnancy (27,29,30), as well as poorer documented health outcomes (30,31) and a more rapid progression to type 2 diabetes (32,33). A recent Australian review reported a greater prevalence of gestational diabetes mellitus (GDM) in Indigenous women, as well as increased rates of adverse outcomes of diabetes in pregnancy, including macrosomia, caesarean section, congenital deformities, low birth weight, hypoglycemia and neonatal trauma (34). These adverse outcomes were greater in rural/remote populations.
Diabetes in Indigenous populations globally is linked to a complex array of factors; however, a common thread is the shared history of colonization (35). The World Health Organization has recognized colonization as the most significant social determinant of health affecting Indigenous peoples worldwide (35). In Canada, this involved: the outlawing of Indigenous gatherings and ceremonies at the end of the nineteenth and throughout the first half of the twentieth centuries; forced community relocations; mandatory residential school attendance where Indigenous languages were forbidden and physical and sexual abuse were common; and discriminatory child welfare legislation that persists today (36). All have undermined Indigenous cultures and values, leading to lasting and intergenerational effects on mental health, family relationships and Indigenous ways of knowing and connecting to the land (37,38). Similar actions were common during the “settlements” of Australia, New Zealand and the United States, with ongoing parallels in chronic disease statistics. It is also essential to realize that the impacts of colonization continue through persisting inequities, exclusion and oppression of Indigenous peoples within Canada.
Other factors contributing to the incidence gap faced by Indigenous peoples include the probable influence of diabetes in pregnancy and the intrauterine milieu (39). Also postulated are possible environmental exposures, such as mercury (40), arsenic (41), polychlorinated biphenyl (PCB) and chlorinated pesticide exposure (42,43). Low levels of vitamin D have also been implicated (44). In addition, genetic vulnerability has been shown to be relevant (45–48), and markers have been studied in Pima Indians in Arizona (49), and are known in the Canadian Ojibway Cree population (50,51). In the Inuit, the TCB1G4 gene leads to a specific kind of type 2 diabetes with abnormal postprandial glucose and normal glycated hemoglobin (A1C); however, there are unclear implications for the role of genetic testing in clinical practice (52).
There is emerging literature on the effect of adverse childhood experiences and subsequent incidence of type 2 diabetes (53,54). In the Indigenous context, stress is accumulative and arises from multiple psychosocial sources (55–58). Poverty is a common experience, which hinders access to needed resources (e.g. healthy foods), as are direct/indirect traumatic experiences resulting from residential schools and child welfare systems (e.g. unresolved grief) (59,60). When stressors operate concurrently, along with living conditions that are overwhelming or chaotic, one's capacity to cope and manage diabetes is undermined. Whether linked to stress or poor dietary patterns, obesity is the most common proximal determinant of diabetes (11,61). One study found “beef and processed foods” to be associated with incident diabetes, whereas “balanced market foods” and “traditional foods” were not predictive, after adjustment for confounders, including waist circumference and adiponectin (62).
The increasing burden of diabetes in Indigenous populations is a major and growing challenge for health systems and Indigenous communities alike, whether First Nations, Inuit or Métis (63). Processes of care have been found to be deficient in 2 large studies in Alberta, associated with greater morbidity and mortality (17,64). A national survey found serious health service challenges for Indigenous populations (65); and a recent review corroborated the survey and suggested there was no best practice evidence out of 17 reviewed Canadian publications between 2008 and 2014 (66). Improving health outcomes would involve ensuring health service quality and equity tailored to the needs of Indigenous peoples with diabetes. This means addressing the social origins of disease and illness located within Indigenous contexts of colonization, inequity and exclusion. New approaches to care are needed that are culturally congruent with Indigenous perspectives and grounded in addressing the impacts of colonization on health that Indigenous peoples continue to experience.
Screening in Indigenous Peoples and/or Communities
Screening and prevention strategies should be implemented in collaboration with community leaders, Indigenous peoples with diabetes, health-care professionals, and funding agencies to engage entire communities, promote environmental changes and prevent increased risk of diabetes in all Indigenous populations, not just rural or remote (67). Such partnerships are important for prioritizing and incorporating local social and cultural contexts, building both trusting relationships and community capacity, enhancing diabetes-related knowledge, and increasing the likelihood of success and sustainment of prevention efforts.
Screening for diabetes in asymptomatic Indigenous adults (>age 18 years) should be considered every 6 to 12 months in those with additional risk factors, especially those with overweight or obesity, those with strong family histories, or women of childbearing age (see Screening for Diabetes in Adults chapter, p. S16), ensuring facilitation of access to clinical care, such that testing can lead to significant follow up action. Regular screening and follow-up is also encouraged in individuals with prediabetes [impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT)], history of GDM, or polycystic ovary syndrome (PCOS), as 20% to 50% of high-risk individuals with IFG may have a 2-hour plasma glucose (PG) ≥11.1 mmol/L (68).
Screening recommendations for Indigenous children and adolescents are outlined in the Type 2 Diabetes in Children and Adolescents chapter, p. S247. As Indigenous children already possess 1 risk factor (high-risk ethnic group), screening for type 2 diabetes should be considered every 2 years, using a combination of an A1C and a fasting plasma glucose (FPG) if they possess ≥2 additional risk factors in non-pubertal children beginning at 8 years of age or ≥1 additional risk factor in pubertal children. Risk factors include obesity; first-degree relative with type 2 diabetes and/or exposure to hyperglycemia in utero, or if they have signs and symptoms of insulin resistance, prediabetes, or use atypical antipsychotic medications (see Recommendation 3. Type 2 Diabetes in Children and Adolescents chapter, p. S251).
Screening has proved possible in both rural and remote communities through appropriate dialogue, respect and planning; with the provision of concomitant health education and care; and the promotion of follow up (26,69–72). In Alberta, substantial numbers of Indigenous individuals with abnormalities have been identified through community-based screening with point-of-care (POC) instruments handled by trained health-care professionals and associated with a quality control program (72). POC A1C screening has shown to be sufficiently accurate as a screening tool for diagnosing diabetes in remote communities (73,74); however, currently, no POC A1C analyzers are approved for the diagnosis of diabetes in Canada (see Monitoring Glycemic Control chapter, p. S47).
While screening with reflectance capillary blood glucose meters is not recommended, it should be noted that it has often happened and continues to happen in community contexts. It is essential that this type of screening be confirmed in a health-care setting. When Indigenous peoples with diabetes are educated on the use of reflectance capillary blood glucose meters, these cautions should be discussed, and infectious disease precautions emphasized.
Retinal photography screening has also been utilized in Canada in remote areas (75), and has been shown to increase the number of screened individuals in Australia (76) (see Retinopathy chapter, p. S210). In the United States, a kidney evaluation program screened 89,552 participants in 49 states, 4.5% of whom were Native American (71).
Depression is associated with type 2 diabetes (77), for which screening and treatment should follow existing best practices. While individuals may benefit from the diagnosis and treatment of depression and other mental health illnesses, cultural approaches may be more appropriate (4,5). Furthermore, several studies have demonstrated associations between greater cultural continuity and better mental health outcomes. Local traditional approaches to wellness around management and support for depression should be explored when appropriate.
Pregnant Indigenous women identified as being at high risk for type 2 diabetes based on clinical risk assessment should be screened with an A1C test at the first antenatal visit to identify pre-existing diabetes (78). For those women with a hemoglobinopathy or renal disease, the A1C test may not be reliable and screening should be performed with an FPG (see Monitoring Glycemic Control chapter, p. S47). If the A1C is ≥6.5% or the FPG is ≥7.0 mmol/L, the woman should be considered to have diabetes in pregnancy and SMBG should start, along with nutritional counselling (see Diabetes and Pregnancy chapter, p. S255). While there is insufficient data on the best tests and their diagnostic interpretation in the early trimester for lower levels of abnormal glycemia, e.g. A1C between 5.7% and 6.4% or FBG between 5.1 and 6.9 mmol/L (see Diabetes and Pregnancy chapter, p. S255), the rationale for screening remains strong, particularly to detect previously undiagnosed type 2 diabetes. However, further research is needed as a recent systematic review pointed out the insufficient evidence regarding cost effectiveness of early testing, as well as information on longer-term benefits (79). If the initial screening is performed before 24 weeks of gestation and is negative, the woman should be re-screened for GDM between 24 to 28 weeks of gestation (see Diabetes and Pregnancy chapter, p. S255). In addition, all women not previously screened for diabetes should be tested between 24 to 28 weeks of gestation.
Postpartum screening after GDM should be carried out between 6 weeks and 6 months, and accompanied with healthy behaviour interventions and ongoing monitoring or treatment (see Diabetes and Pregnancy chapter, p. S255). To date, rates of postpartum OGTT screening have been shown to be low, indicating that new approaches may be required to account for challenges among women with a new baby to find time to do screening tests, let alone capacity to do so while breastfeeding. Such challenges support the case for A1C and random or fasting glucose, POC testing, and messages that emphasize the benefit of delaying disease onset rather than diagnosing a condition that may be felt by affected women to be “expected and assumed” (80,81).
Primary Prevention
Prevention of type 2 diabetes in those with identified prediabetes (IGT/ IFG) is now an established desired practice (82,83). Proven interventions include healthy behaviour changes and regular physical activity that induce moderate weight loss. Metformin may also be used (see Reducing the Risk of Developing Diabetes chapter, p. S20). The Diabetes Prevention Program from the United States was effective for all ethnicities, but the extent to which it can be applied in Canadian Indigenous contexts is unknown. Primary prevention approaches within Indigenous communities have been undertaken in Canada by the Aboriginal Diabetes Initiative (ADI) (84) and have focused on common risk factors, including obesity, sedentary lifestyle and unhealthy diet, as well as through interventions aimed at increasing health literacy and access to physical activity. Community involvement in developing the intervention and framing the intervention within Indigenous cultural perspectives have been variable. Results of the ADI are unknown. A study with Algonquin women sought to understand the cultural factors that would likely impact the prevention of diabetes, identifying the following factors: the importance of family and social ties; the possibility of preserving cultural values; the opportunity to learn behaviours through educational resources adapted to needs and culture; the possibility of saving money through better diet and access to self-monitoring of blood glucose (SMBG) supplies (85).
In Arizona, 95 men and women with obesity and normoglycemia between the ages of 25 to 54 years were randomized to treatments named “Pima Action” (Action) and “Pima Pride” (Pride) and followed for 12 months. “Action” involved structured activity and nutrition interventions; and “Pride” included unstructured activities, emphasizing Pima history and culture. Action members gained more weight and had higher BG levels at the end of the study, suggesting that less structured and more culturally-grounded interventions may be more relevant and successful (86). More recently, a prevention study in 3,135 participants in 36 Indigenous communities in the United States showed baseline psychosocial characteristics of family support and psychological distress predicted favourable baseline weight and weight change post-intervention, while coping skills and trauma exposure did not (87).
In light of the disproportionate burden of diabetes, appropriate population level prevention approaches are critical investments. Nevertheless, it remains unclear whether increased knowledge and awareness, or increased community physical activity resources fill a gap created by structural barriers from social inequities and colonization. Prevention should be critically informed by the social contexts that shape the health of Indigenous peoples, as well as resourced to ensure effectiveness and sustainability. For example, the United States-based Traditional Foods Project aimed to increase access to traditional foods, physical activity and social support (88). Indigenous communities across the country applied their traditional ecological knowledge, specific to the history and culture of their tribe, to protect their communities' land, languages, culture, memory and traditional food practices. Sharing and documenting food sovereignty was a priority. A collection of stories told by tribes about their traditional foods systems was published on the Native Diabetes Wellness Program website. Underpinning the stories are long-sighted lessons for sustainability, embedded in cultural significance and emotional attachment, and inspired by agency (i.e. capacity of acting or of exerting power), self-determination, and hope, for the health of the people (89).
Type 2 diabetes in Indigenous youth is the fastest growing pediatric chronic disease worldwide (16), with childhood obesity as the immediate determinant. The latest Cochrane review of prevention efforts with respect to childhood obesity indicated the following to be promising policies and strategies: school curriculum that includes healthy eating, physical activity and positive body image; increased sessions for physical activity and the development of fundamental movement skills throughout the school week; improvements in nutritional quality of the food supply in schools; environments and cultural practices that support healthy eating and physical activity throughout the day for children; teacher/staff support to implement health promotion strategies and activities (e.g. professional development, capacity-building activities); and parent support and home activities that encourage children to be more active, eat more nutritious foods, and spend less time in screen-based activities (90). While many of these measures have been applied in the Indigenous context, studies have been small, designs have been disparate and the degree of engagement with the community has been variable (91). Two prime examples in Canada were carried out in Kahnawake and Sandy Lake, where broad community-based participatory research projects were conducted (67,92). Although unpublished, “Drop the Pop” campaigns have taken hold in various communities. Similarly, the Traditional Foods Project's partners offered insight to the Bureau of Indian Education in the United States, as they developed their School Health and Wellness Policy supporting the provision for “healthy traditional and cultural foods”. Tribal schools also are providing hands-on learning activities about growing healthy foods. Sustainability of these activities is strengthened by local and national efforts, including the “Farm to School” initiative (93).
In the United States, Zuni First Nations children who received an educational component targeting decreased consumption of sugared beverages, knowledge of diabetes risk factors, and access to a youth-oriented fitness centre demonstrated significantly decreased insulin resistance (94). These types of interventions aimed at decreasing childhood obesity, as well as efforts to promote breastfeeding in the first year of life (95), may help to reduce the risk for diabetes in Indigenous youth.
Finally, pregnancy provides an optimal window of opportunity for intervention to reduce long-term risk for both mothers and offspring. Strategies aimed at the prevention of pre-gravid obesity prior to first conception or subsequent pregnancy may be important tools to decrease the incidence of GDM (96) and type 2 diabetes in pregnancy, thereby potentially decreasing the incidence of diabetes in subsequent generations of Indigenous peoples (39).
Management
Similar to prevention strategies, management of diabetes with Indigenous peoples should incorporate the social and cultural contexts of the community from which the person originates, while also adhering to current clinical practice guidelines (66). One pilot study with a wait-list control group in Native Hawaiians showed that culturally adapted diabetes self-management education building on culturally relevant knowledge and activities (i.e. group-based educational format to facilitate social support, convenient community location, delivered by local community members in the local language, incorporation of local images/food/common physical activities/local people to increase relevance) for 3 months improved A1C, diabetes understanding and diabetes self-management (97,98). In a qualitative study in rural Australia, participants reported both negative influences (i.e. poor access to culturally appropriate health services, dislocation from cultural support systems, exposure to racism, poor communication with health-care professionals and economic hardship) and positive influences (i.e. cultural and traditional knowledge) that affected their health and well-being (99). Participants said that while they often felt overwhelmed and confused by the burden of chronic illness, they drew strength from being part of an Indigenous community, having regular and ongoing access to primary health care, and being well-connected to a supportive family network. Within this context, elders played an important role in increasing people's awareness of the impact of chronic illness on people and communities (99). Another qualitative study conducted with Canadian urban First Nations suggested they and their caregivers struggled with balancing two worlds, accessing care, and dealing with diabetes from cultural and emotional perspectives (100). A recent study of health-care experiences among Indigenous people with type 2 diabetes highlights the perpetuation of inequalities in care from a sample drawn from 5 Indigenous communities in 3 Canadian provinces (101). While service providers were identified as capable of mitigating potential for harm through engaging with patients' social worlds, a corresponding analysis of physician experiences of providing care to Indigenous peoples with type 2 diabetes highlights structural barriers undermining capacity to shift clinical relationships (102). A recent analysis of a well-established program in Northern Québec showed that Indigenous peoples with diabetes had frequent contacts with the system, but gaps in the management of complications (103). Finally, a recent systematic review found that multiple system-level approaches are required in the delivery of health-care for diabetic foot disease in Indigenous peoples (104).
While most diabetes education programs work most effectively when delivered by interprofessional teams, in Indigenous communities, where access to physicians and other critical allied health professionals is often limited, strategies to improve care should focus on building capacity of existing health-care providers (e.g. community health-care providers, nurses to implement clinical practice guidelines) (26,105–107). A diabetes/chronic disease management program in a Hawaiian/Samoan Indigenous population successfully incorporated self-management and patient education to address nutrition and exercise, utilizing community health workers in the application of clinical practice guidelines. The study demonstrated a significant improvement in A1C levels and patient knowledge of reducing consumption of unhealthy foods (108). Maori and Pacific Islander adults with type 2 diabetes and CKD received community care provided by local health-care assistants to manage hypertension and demonstrated a reduction in systolic blood pressure (BP) and in 24-hour urine protein, and a greater number of prescribed antihypertensives; left ventricular mass and left atrial volume progressed in the usual care group, but not in the intervention group (109).
Regarding cost-effectiveness, a systematic review of primary care initiatives in Indigenous adult populations in Canada, Australia, New Zealand and the United States examined increased funding, system-level initiatives and single service components, concluding that the literature in this area was insufficient to make recommendations (110). Of 2,714 publications, only 13 met the authors' inclusion criteria (interventions aimed at improving the health system, clinic system or service level), and only 6 showed improvements in surrogate outcomes. The review highlighted the general reliance on intermediate health outcomes and observational studies, and stressed the need for larger, more rigorous studies with more robust outcomes of interest (i.e. hospitalizations, mortality) to support policy and practice recommendations (110).
Multifaceted clinical organizational and team-based interventions that have suggested benefit include: diabetes registries, recall systems, care plans and training for community health workers, and outreach services. Despite the effectiveness of multifaceted interventions, key elements are unclear (111–113) and the economic effectiveness is undetermined (114). Two newer Australian studies show that cycles of quality improvement that focus on organizational systems improve processes of care in pregnant women (115), as well as in-care processes and some surrogate outcomes in type 2 diabetes (116). Quality improvement processes with community-driven initiatives have demonstrated improvements in A1C testing from 41% to 72%, with an increase in the proportion of people at target A1C (<7.0%) from 19% to 28% (113). In Canada, provincial and federal government-led quality improvement projects have demonstrated improvements in type 2 diabetes outcomes in non-Indigenous settings (117–119). Indigenous-specific project funding is needed to examine the impact of community-driven quality improvement initiatives that are rooted in a cultural lens and prioritize community needs, resources and policies. Finally, management of diabetes in women in the child-bearing years should focus on the identification and optimal treatment of pre-existing (undiagnosed) diabetes as it is commonly missed and has been associated with poor outcomes, including an increased risk for stillbirth (30,120).
E4E Vignette:
Dorothy is a 55-year-old female from a reserve adjacent to your rural practice. She has attended your clinic over the years for her general health needs and, most recently, for hypertension. She has booked to see you because she is concerned she has diabetes. Dorothy has a strong family history of diabetes and mentions that a close friend was recently quite ill and diagnosed as well. Dorothy has symptoms of diabetes, so you send her for bloodwork, confirming the diagnosis.
You call her back to the clinic to inform Dorothy of this diagnosis and the need for her to begin self-monitoring of her blood glucose in order to determine appropriate treatment. As expected, she is upset about the news but quickly settles, so you begin to provide your usual brief overview of diabetes, self-monitoring approach, and management tips. You summarize by encouraging her to eat well and exercise. She agrees to your offer of a referral for more diabetes education. You provide a prescription for a glucose meter and ask her to book an appointment with you in a few weeks.
Nine months later, Dorothy returns for a refill of her antihypertensive medications and to re-engage about the diagnosis of diabetes. You realize she did not follow up from her last visit, which is quite similar to your other Indigenous patients. You inquire, and Dorothy reveals that she was so upset and overwhelmed with the delivery of the diabetes diagnosis and your subsequent approach during the last visit, that she went into denial. You are surprised because you felt that the appointment went well and that your summary and plan were clear and concise.
For moving forward at this critical moment within the clinical interaction, aspects of the care framework are highlighted:
Dorothy indicated that she was upset and overwhelmed by you during the last visit. Pertinent to this discord, the care framework suggests that health-care providers “Become aware of and explore moments of discord, paying particular attention to patient resistance, hesitation and withdrawal, which possibly arise from tensions in historical relationships.” You do so by asking about what upset and overwhelmed her about your approach. She hesitates but eventually explains that she feels as though you do not always care about her concerns, that you see her as taking up your precious time. She also adds that when you recommended she eat more vegetables, like carrots, it made her remember an experience in residential school, where a residential school worker once locked her in a cell in which all she had to eat for three days was a single carrot. She says that when she had tried to speak up, she felt you spoke over her, so was unable to communicate her anxieties. The practice tips indicated above and E4E culture-based strategies in the table offer guidance for an enhanced health-care provider response.
Because you acknowledged your role causing Dorothy to withdraw from the interaction, Dorothy seems more at ease and states she is ready to focus on addressing her diabetes. The care framework suggests that health-care providers explore social contexts that may influence diabetes, and so you enquire about social resource limitations in her life and adverse life experiences that may be factors. She asks why, and then explains that she is her grandchildren's primary caregiver, depended on by many people but without anyone to turn to for her own support. She also speaks about her fear of losing her job due to a hostile work environment in which even taking time off to visit the doctor is difficult. You share that those factors cause stress and are known in the research to diminish her resilience and often become barriers to health. The care framework recommends that acknowledging the impacts of these social factors and identifying patient priorities are important steps at this phase. You do so, naming concepts of effort-reward imbalance (123) and lateral violence (124). These resonate with her, and she asks for tips to address these in her life, to work on together with her diabetes.
Educating for Equity (E4E) Care Framework
Much of the above literature indicates that the context of traditions, language and culture could play an important role in the care physicians provide, since usual approaches have had limited effect. Emerging evidence from an international research team, Educating for Equity (121), indicates that diabetes management should more directly focus on social and cultural aspects specific to Indigenous populations. The E4E framework guides physicians in addressing social and cultural domains in their clinical interactions with patients. Core directives guide providers to: ensure reciprocal relationships, recognize the diversity of patients, provide care specific to each patient's needs, support them in developing capacity for addressing social determinants of health, and respect patient priorities. These are embedded within a set of principles that recognize colonization as the predominant cause of health inequities for Indigenous peoples, health care equity as about providing appropriate resources according to need, and empowerment focused on building capacity with patients to address social drivers of disease. Within the framework, social factors (e.g. poverty, discrimination) are positioned as patient barriers to improved diabetes outcomes, while cultural factors facilitate improved clinical relationships and patient capacity. The framework, therefore, provides a lens to understand, identify and apply opportunities for augmenting patient capacity for change. As authors, we emphasize the relevance of this framework and, therefore, provide a synopsis and clinical vignette within this chapter in order to aid clinicians to explore its possibilities for clinical practice. Readers are invited to access E4E publications for more in-depth information around the evidence and consultation process supporting the framework (Table 1
Improving diabetes outcomes for Indigenous peoples with diabetes includes the need for organizational enhancements and team-based approaches, but is limited by the reality of health-care human resources in many Indigenous communities. Health-care personnel gaps appear to be filled by expanding the roles of existing front-line staff. While prevention strategies must consider cultural elements and the influence of inequities on diabetes outcomes, so too must clinical service. The following section provides a description of an approach to care that integrates key aspects of the complex associations between cultural contexts and social inequities that frame diabetes within Indigenous populations.
| Table 1 Educating for Equity (E4E) Clinical Strategies |
|
|---|---|
| A1C, glycated hemoglobin; SMBG, self-monitoring of blood glucose. | |
| E4E Strategies for addressing social barriers to improve diabetes outcomes: |
|
Social & economic resource disparities
Accumulation of adverse life experiences
Colonization, inequity and health care
|
|
| Educating for Equity Strategies for facilitating outcomes using a cultural approach: |
|
Culture is therapeutic
Culture informs relationships
Culture frames knowledge
|
|
Social Barriers to Desired Diabetes Outcomes
Understanding social factors that influence diabetes of Indigenous populations assists health-care providers in providing care that: 1) addresses barriers to desired diabetes outcomes; 2) better achieves management/therapeutic goals; and 3) fosters self-efficacy and health with patients.
Social and economic resource disparities
Material deprivation within the social environment directly impacts diabetes. Relationships between resource limitations, socioeconomic status, and the social environment directly impact diabetes through material deprivation. Indirectly, psychosocial pathways, such as stress, depression, anxiety and loss of control, further undermine health outcomes. This requires health-care providers to recognize socioeconomic disadvantage as a normalized state for many Indigenous peoples, limiting choices, increasing levels of stress, and diminishing capacity for self-care and lifestyle change. Attention for limited resources among families is key to recognizing the contexts in which self-care occurs. Limited budgets for food and financial sharing result in the diversion of resources, making family an important source of support as well as a key stressor.
Accumulation of adverse life experiences
Persistent and recurring experiences of adversity accumulate, influencing wellness and health. These diminish resilience and capacity to cope with disease. Health-care providers should keep in mind that adversity and support are complex and often ambiguous. The impact of residential schools not only persists among traumatized individuals, but the system continues to adversely influence health behaviours that impact others.
Colonization, inequity and health care
Given the context of historical relationships, social exclusion and trauma experienced by Indigenous persons, clinical approaches that establish physician authority, expertise, status and professional distance can negatively impact physician-patient relationships. Health-care providers should recognize unequal treatment as a reality in Canada's health system. This plays out for Indigenous peoples in heightened awareness and reaction when power and authority are expressed in the physician-patient relationship.
Facilitating Outcomes Using a Cultural Approach
Viewing culture as a protective mechanism involves moving beyond envisioning Indigenous peoples' experience of health and illness from the patient's cultural lens alone, in order to understand and support a patient's own preferences and connections to cultural resources.
Culture is therapeutic
As health is positively correlated with a sense of security in cultural identity, accessing cultural knowledge and traditions means that culture is protective for many Indigenous peoples. While Indigenous peoples vary in how they connect with traditional worldviews, traditional medicine and ceremony are widely desired for accessing and re-connecting to culture in conjunction with Western medicine. Many Indigenous people do not talk about traditional medicines or practices with health-care providers, possibly due to incongruence between these knowledge systems, as well as persistent mistrust and fear of reprisal from health-care providers.
Culture informs relationships
Cultural perspectives inform how patients experience diabetes and engage with health care. Patient resistance may reflect the need for health-care providers to focus on relationship-building strategies. Patients and health-care providers have a mutual interest in getting to know one another better. Health-care providers who pay attention to issues of process and pace can help patients meet their desire to be treated with respect and without judgment; it can also allow health-care providers to move toward safer and more inviting environments that foster sharing. An Indigenous person's experiences of diabetes and its care are also embedded in connectedness to others, particularly family dynamics and community supports and structures, of which patient-provider relationships and interprofessional health-care teams are a part.
Culture frames knowledge
Through contextualization and exchange between health-care providers and patients, greater attention can be paid to reaching mutual understanding. Failing to elicit and address the patient's social and cultural contextual factors silences patient perspective and eliminates opportunity to ground clinical management approaches within a patient-centred approach, potentially exacerbating negative outcomes. Limitations of diabetes and general health literacy stemming from inadequate access to education may hinder the Indigenous person's abilities to engage with health and diabetes management recommendations. Conversely, placing diabetes care knowledge within the cultural, social and political landscape of Indigenous peoples can facilitate patient engagement with accessing diabetes knowledge. Effective communication for achieving knowledge exchange and patient education integrates intercultural communication strategies.
It is not acceptable to presume that Indigenous people are uninterested in the physiology of diabetes when, in reality, they report wanting to understand what causes diabetes and how to manage the illness. Health-care providers need to recognize stressors that adversely impact learning, draw on sources of health information actually available to patients (in professional, popular and folk realms) (122), mitigate resistance to health information due to health-care provider–patient relationship discord, and foster modes of knowledge transmission appropriate for the social and cultural context.
Key Concepts for Application of the E4E Care Framework
Patient-centred care (125), cultural competency and cultural safety (126) appear to be critical for quality care with Indigenous peoples, but are also broad concepts that require interpretation. The E4E framework posits that improving health outcomes for Indigenous peoples involves addressing historical and contextual factors in which disease and illness occur, while healing distrust in the Canadian health-care system. This moves beyond merely defining cultural competency as a list of patient beliefs and behaviours for clinicians, toward structural competency (127) that requires critical consciousness of social factors driving disease and wellness. It also highlights the fundamental role of anti-racism in the equitable delivery of health care (128,129). On top of these are layered notions of authentic inclusion grounded in Indigenous cultural approaches, moving providers toward vital relational and culturally-informed aspects of care that enable the facilitation of improved diabetes outcomes.
The E4E framework provides knowledge and recommendations for use as a motivational interviewing (130) approach within the clinical interaction that unpacks the described complex concepts. This approach aims to leverage patient motivation for health promoting behaviour change, among other things by engaging “open-ended questions, reflective listening, and support for patient autonomy and self-efficacy” (130) to overcome ambivalence, resistance and avoidance around disease management. As described in the E4E vignette, patient engagement is facilitated by screening for resource limitations influencing diabetes onset, as well as exploring with patients their perspectives on adversities that undermine one's capacity to manage diabetes. Notably, trauma informed relational work (131) that seeks to address power imbalance, authoritarian approaches and a history of mistrust is the critical first step that enables patient engagement.
Recommendations
- Management of prediabetes and diabetes in Indigenous populations should follow the same clinical practice guidelines as those for the general population with respect for, and sensitivity to, particular social, historical, economic, cultural and geographic issues as they relate to diabetes care and education [Grade D, Consensus].
- Starting in early childhood, Indigenous individuals should be evaluated for modifiable risk factors of diabetes (e.g. obesity, inactivity, unhealthy diet), prediabetes or metabolic syndrome [Grade D, Consensus] (see Type 2 Diabetes in Children and Adolescents chapter, p. S247).
- Screening for diabetes in Indigenous populations should follow guidelines for high-risk populations (i.e. younger, including children, and at more frequent intervals depending on presence of additional risk factors) [Grade D, Consensus] (see Screening for Diabetes in Adults chapter, p. S16; Type 2 Diabetes in Children and Adolescents chapter, p. S247.
- To promote access to screening for remote Indigenous populations, access to standard laboratory testing is recommended; in its absence, point of care testing for A1C may be considered where testing is associated with a quality control program; and interpretation and follow-up expertise is available [Grade D, Consensus].
- Retinal photography screening programs may be used in Indigenous communities living in remote areas to promote access to screening [Grade B, Level 2 (76)] (see Retinopathy chapter, p. S210).
- Attainment of a healthy body weight prior to conception should be promoted among Indigenous women to reduce their risk for GDM [Grade D, Consensus]. Nutrition counseling should be provided on healthy eating and prevention of excessive weight gain in early pregnancy, ideally before 15 weeks of gestation, to reduce the risk of GDM [Grade D, Consensus] (see Diabetes and Pregnancy chapter, p. S255).
- Indigenous women identified as being at risk for type 2 diabetes who are planning a pregnancy should:
- Be screened for diabetes using FPG and/or A1C [Grade D, Consensus] (see Screening for Diabetes in Adults chapter, p. S16).
- If identified as having diabetes, receive preconception counseling that includes optimal diabetes management, including nutrition and physical activity advice, preferably in consultation with an interprofessional pregnancy team to optimize maternal and neonatal outcomes [Grade D, Consensus] (see Diabetes and Pregnancy chapter, p. S255).
- Pregnant Indigenous women identified as being at risk for type 2 diabetes should:
- Be offered screening with an A1C test at the first antenatal visit, if not screened preconception [Grade D, Consensus] (see Diabetes and Pregnancy chapter, p. S255].
- Pregnant Indigenous women with diabetes should:
- Receive management following the same clinical practice guidelines as those for the general population to improve pregnancy outcomes [Grade D, Consensus].
- Postpartum:
- Indigenous women with pre-existing diabetes or GDM should be encouraged to breastfeed immediately to reduce the risk of neonatal hypoglycemia [Grade D, Consensus] (see Diabetes and Pregnancy chapter, p. S255).
- The infant of a pregnant Indigenous woman with diabetes should receive close monitoring for neonatal hypoglycemia with capillary blood glucose monitoring for up to 36 hours [Grade D, Consensus].
- Indigenous women with GDM should be screened with a 75 g OGTT between 6 weeks and 6 months postpartum to detect prediabetes and diabetes [Grade D, Consensus] (see Diabetes and Pregnancy chapter, p. S255)] and regularly thereafter according to recommendations in Screening for Diabetes in Adults chapter, p. S16].
- Indigenous communities should be supported in initiating and maintaining culturally appropriate primary prevention programs for children and adults to assess and mitigate risk factors such as:
- Geographic and cultural barriers [Grade D, Consensus]
- Food insecurity [Grade D, Consensus]
- Psychological stress [Grade D, Consensus]
- Insufficient infrastructure [Grade D, Consensus]
- Settings that are not conducive to physical activity [Grade D, Consensus]
Abbreviations:
A1C, glycated hemoglobin; ADI, Aboriginal Diabetes Initiative; BG, blood glucose; BP, blood pressure; CV, cardiovascular; CKD, chronic kidney disease; ESRD, end stage renal disease; GDM, gestational diabetes; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; PCOS, polycystic ovary syndrome; POC, point of care.
Other Relevant Guidelines
- Screening for Diabetes in Adults, p. S16
- Reducing the Risk of Developing Diabetes, p. S20
- Organization of Diabetes Care, p. S27
- Monitoring Glycemic Control, p. S47
- Weight Management in Diabetes, p. S124
- Cardiovascular Protection in People with Diabetes, p. S162
- Treatment of Hypertension, p. S186
- Chronic Kidney Disease in Diabetes, p. S201
- Retinopathy, p. S210
- Foot Care, p. S222
- Type 2 Diabetes in Children and Adolescents, p. S247
- Diabetes and Pregnancy, p. S255
Related Websites
First Nation, Inuit and Aboriginal Health. http://www.hc-sc.gc.ca/fniah-spnia/diseases-maladies/diabete/index-eng.php. Accessed March 21, 2017.
National Aboriginal Diabetes Association. http://www.nada.ca. Accessed March 21, 2017.
Literature Review Flow Diagram for Chapter 38: Type 2 Diabetes and Indigenous Peoples
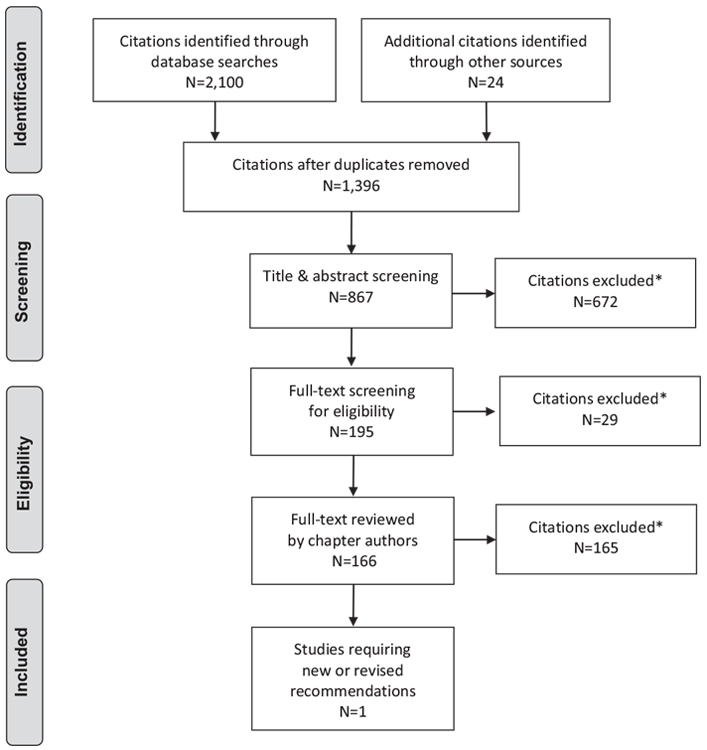
*Excluded based on: population, intervention/exposure, comparator/control or study design.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097 (132).
For more information, visit www.prisma-statement.org.
Author Disclosures
No authors have anything to disclose.
References
- Richmond CA, Ross NA. The determinants of First Nation and Inuit health: A critical population health approach. Health Place 2009;15:403–11.
- Maar MA, Manitowabi D, Gzik D, et al. Serious complications for patients, care providers and policy makers: Tackling the structural violence of First Nations people living with diabetes in Canada. Int Indigenous Policy J 2011;21:http://ir.lib.uwo.ca/iipj/vol2/iss1/6. Article 6.
- Jacklin KM, Henderson RI, Green ME, et al. Health care experiences of Indigenous people living with type 2 diabetes in Canada. CMAJ 2017;189:E106–12.
- Chandler MJ, Lalonde C. Cultural continuity as a protective factor against suicide in First Nations Youth. Horizons 2008;10:68–72.
- Oster RT, Grier A, Lightning R, Mayan MJ, Toth EL. Cultural continuity, traditional Indigenous language, and diabetes in Alberta First Nations: A mixed methods study. Int J Equity Health 2014;13:92. doi:10.1186/s12939-014-0092-4.
- Truth and Reconciliation Commission of Canada. Truth and reconcilliation commission of Canada: calls to action. Winnipeg, MB: Truth and Reconciliation Commission of Canada 2012. 2015. http://www.trc.ca/websites/trcinstitution/File/2015/Findings/Calls_to_Action_English2.pdf.
- Yu CH, Zinman B. Type 2 diabetes and impaired glucose tolerance in aboriginal populations: A global perspective. Diabetes Res Clin Pract 2007;78:159–70.
- Gracey M, King M. Indigenous health part 1: Determinants and disease patterns. Lancet 2009;374:65–75.
- Chronic Disease Surveillance and Monitoring Division, Centre for Chronic Disease Prevention and Control. Diabetes in Canada: Facts and figures from a public health perspective. Ottawa, ON: Public Health Agency of Canada, 2011 http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/index-eng.php.
- Turin TC, Saad N, Jun M, et al. Lifetime risk of diabetes among first nations and non-first nations people. CMAJ 2016;188:1147–53.
- Singer J, Putulik Kidlapik C, Martin B, et al. Food consumption, obesity and abnormal glycaemic control in a Canadian Inuit community. Clin Obes 2014;4:316– 23.
- Oster RT, Johnson JA, Balko SU, et al. Increasing rates of diabetes amongst status Aboriginal youth in Alberta, Canada. Int J Circumpolar Health 2012;71: 1–7.
- Jiang Y, Osgood N, Lim HJ, et al. Differential mortality and the excess burden of end-stage renal disease among First Nations people with diabetes mellitus: A competing-risks analysis. CMAJ 2014;186:103–9.
- Dyck RF, Hayward MN, Harris SB, et al. Prevalence, determinants and co-morbidities of chronic kidney disease among First Nations adults with diabetes: Results from the CIRCLE study. BMC Nephrol 2012;13:57.
- Komenda P, Lavallee B, Ferguson TW, et al. The prevalence of CKD in rural Canadian Indigenous peoples: Results from the First Nations community based screening to improve kidney health and prevent dialysis (FINISHED) screen, triage, and treat program. Am J Kidney Dis 2016;68:582–90.
- Dean HJ, Sellers EA. Children have type 2 diabetes too: An historical perspective. Biochem Cell Biol 2015;93:425–9.
- Maple-Brown LJ, Sinha AK, Davis EA. Type 2 diabetes in indigenous Australian children and adolescents. J Paediatr Child Health 2010;46:487– 90.
- Dyck RF, Jiang Y, Osgood ND. The long-term risks of end stage renal disease and mortality among First Nations and non-First Nations people with youth-onset diabetes. Can J Diabetes 2014;38:237–43.
- Harris SB, Naqshbandi M, Bhattacharyya O, et al. Major gaps in diabetes clinical care among Canada’s First Nations: Results of the CIRCLE study. Diabetes Res Clin Pract 2011;92:272–9.
- Martens PJ, Bartlett J, Burland E, et al. Profile of metis health status and healthcare utilization in Manitoba: a population-based study. Winnipeg: University of Manitoba: Policy MCfH. 2010. http://mchp-appserv.cpe.umanitoba.ca/reference/MCHP-Metis_Health_Status_Full_Report_(WEB)_(update_aug11_2011).pdf.
- Martens PJ, Martin BD, O’Neil JD, et al. Diabetes and adverse outcomes in a First Nations population: Associations with healthcare access, and socioeconomic and geographical factors. Can J Diabetes 2007;313:223–32.
- Chuback J, Embil JM, Sellers E, et al. Foot abnormalities in Canadian Aboriginal adolescents with type 2 diabetes. Diabet Med 2007;24:747–52.
- Rose G, Duerksen F, Trepman E, et al. Multidisciplinary treatment of diabetic foot ulcers in Canadian Aboriginal and non-Aboriginal people. Foot Ankle Surg 2008;14:74–81.
- Ross SA, McKenna A, Mozejko S, et al. Diabetic retinopathy in native and nonnative Canadians. Exp Diabetes Res 2007;2007:76271.
- Naqshbandi M, Harris SB, Esler JG, et al. Global complication rates of type 2 diabetes in Indigenous peoples: A comprehensive review. Diabetes Res Clin Pract 2008;82:1–17.
- Oster RT, Toth EL. Differences in the prevalence of diabetes risk-factors among First Nation, Metis and non-Aboriginal adults attending screening clinics in rural Alberta, Canada. Rural Remote Health 2009;9:1170.
- Dyck R, Osgood N, Lin TH, et al. Epidemiology of diabetes mellitus among First Nations and non-First Nations adults. CMAJ 2010;182:249–56.
- Oster RT, Johnson JA, Hemmelgarn BR, et al. Recent epidemiological trends among status Aboriginal adults. CMAJ 2011;183:E803–8.
- Aljohani N, Rempel BM, Ludwig S, et al. Gestational diabetes in Manitoba during a twenty-year period. Clin Invest Med 2008;31:E131–7.
- Oster RT, King M, Morrish DW, et al. Diabetes in pregnancy among First Nations women in Alberta, Canada: A retrospective analysis. BMC Pregnancy Childbirth 2014;14:
- Oster RT, Toth EL. Longitudinal rates and risk factors for adverse birth weight among First Nations pregnancies in Alberta. J Obstet Gynaecol Can 2016;38:29–34.
- Shen GX, Shafer LA, Martens PJ, et al. Does First Nations ancestry modify the association between gestational diabetes and subsequent diabetes: A historical prospective cohort study among women in Manitoba, Canada. Diabet Med 2015;33:1245–52.
- Chamberlain CR, Oldenburg B, Wilson AN, et al. Type 2 diabetes after gestational diabetes: Greater than fourfold risk among Indigenous compared with non-Indigenous Australian women. Diabetes Metab Res Rev 2016;32:217–27.
- Duong V, Davis B, Falhammar H. Pregnancy and neonatal outcomes in Indigenous Australians with diabetes in pregnancy.World J Diabetes 2015;6:880–8.
- Cunningham M. Chapter V: Health. In United Nations, Permanent Forum on Indigenous Issues, State of the world’s Indigenous peoples. New York: United Nations, 2009:156–87.
- Canadian Human Rights Tribunal: Hearing before the First Nations Child and Family caring, Society of Canada, Assembly of First Nations, Canadian Human Rights Commission, Attorney General of Canada, Chiefs of Ontario, Amnesty International. 2016.
- Allan B, Smylie J. First peoples, second class treatment. The role of racism in the health and well-being of Indigenous peoples in Canada. Toronto:Well Living House for Wellesley Institute. 2015. http://www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf. Accessed January 19, 2018.
- Protudjer JL, Dumontet J, McGavock JM. My voice: A grounded theory analysis of the lived experience of type 2 diabetes in adolescence. Can J Diabetes 2014;38:229–36.
- Osgood ND, Dyck RF, Grassmann WK. The inter- and intragenerational impact of gestational diabetes on the epidemic of type 2 diabetes. Am J Public Health 2011;101:173–9.
- Jeppesen C, Valera B, Nielsen NO, et al. Association between whole blood mercury and glucose intolerance among adult Inuit in Greenland. Environ Res 2015;143(Pt A):192–7.
- Navas-Acien A, Silbergeld EK, Streeter RA, et al. Arsenic exposure and type 2 diabetes: a systematic review of the experimental and epidemiologic evidence. Environ Health Perspect 2006;114:641–8.
- Aminov Z, Haase R, Carpenter DO. Diabetes in Native Americans: Elevated risk as a result of exposure to polychlorinated biphenyls (PCBs). Rev Environ Health 2016;31:115–19.
- Pal S, Blais JM, Robidoux MA, et al. The association of type 2 diabetes and insulin resistance/secretion with persistent organic pollutants in two First Nations communities in Northern Ontario. Diabetes Metab 2013;39:497–504.
- Mansuri S, Badawi A, Kayaniyil S, et al. Associations of circulating 25(OH)D with cardiometabolic disorders underlying type 2 diabetes mellitus in an Aboriginal Canadian community. Diabetes Res Clin Pract 2015;109:440–9.
- Bian L, Hanson RL, Ossowski V, et al. Variants in ASK1 are associated with skeletal muscle ASK1 expression, in vivo insulin resistance, and type 2 diabetes in Pima Indians. Diabetes 2010;59:1276–82.
- Bian L, Hanson RL, Muller YL, et al. Variants in ACAD10 are associated with type 2 diabetes, insulin resistance and lipid oxidation in Pima Indians. Diabetologia 2010;53:1349–53.
- Degaffe GH, Vander Jagt DL, Bobelu A, et al. Distribution of glyoxalase I polymorphism among Zuni Indians: The Zuni Kidney Project. J Diabetes Complications 2008;22:267–72.
- Voruganti VS, Cole SA, Ebbesson SO, et al. Genetic variation in APOJ, LPL, and TNFRSF10B affects plasma fatty acid distribution in Alaskan Eskimos. Am J Clin Nutr 2010;91:1574–83.
- Muller YL, Piaggi P, Hanson RL, et al. A cis-eQTL in PFKFB2 is associated with diabetic nephropathy, adiposity and insulin secretion in American Indians. Hum Mol Genet 2015;24:2985–96.
- Hegele RA, Cao H, Harris SB, et al. Hepatocyte nuclear factor-1 alpha G319S. A private mutation in Oji-Cree associated with type 2 diabetes. Diabetes Care 1999;223:524.
- Hegele RA, Zinman B, Hanley AJ, et al. Genes, environment and Oji-Cree type 2 diabetes. Clin Biochem 2003;36:163–70.
- Manousaki D, Kent JW, Haack K, et al. Toward precision medicine: TBC1D4 disruption is common among the inuit and leads to underdiagnosis of type 2 diabetes. Diabetes Care 2016;39:1889–95.
- Huffhines L, Noser A, Patton SR. The link between adverse childhood experiences and diabetes. Curr Diab Rep 2016;16:54.
- Huang H, Yan P, Shan Z, et al. Adverse childhood experiences and risk of type 2 diabetes: A systematic review and meta-analysis. Metabolism 2015;64:1408–18.
- Rock M. Sweet blood and social suffering: Rethinking cause-effect relationships in diabetes, distress, and duress. Med Anthropol 2003;22:131–74.
- Willis E, Pearce M, McCarthy C, et al. Utility stress as a social determinant of health: Exploring the links in a remote Aboriginal community. Health Promot J Austr 2006;17:255–9.
- Adelson N. The embodiment of inequity: Health disparities in aboriginal Canada. Can J Public Health 2005;96(Suppl. 2):S45–61.
- Currie CL, Wild TC, Schopflocher DP, et al. Racial discrimination, post traumatic stress, and gambling problems among urban aboriginal adults in Canada. J Gambl Stud 2013;29:393–415.
- Howard HA. Canadian residential schools and urban indigenous knowledge production about diabetes. Med Anthropol 2014;33:529–45.
- Smye V, Browne AJ, Varcoe C, et al. Harm reduction, methadone maintenance treatment and the root causes of health and social inequities: An intersectional lens in the Canadian context. Harm Reduct J 2011;8:17.
- Hu H, Huff CD, Yamamura Y, et al. The relationship between Native American ancestry, body mass index and diabetes risk among Mexican-Americans. PLoS ONE 2015;10.
- Reeds J, Mansuri S, Mamakeesick M, et al. Dietary patterns and type 2 diabetes mellitus in a First Nations community. Can J Diabetes 2016;40:304– 10.
- Foulds HJ, Shubair MM, Warburton DE. A review of the cardiometabolic risk experience among Canadian Metis populations. Can J Cardiol 2013;29:1006–13.
- Campbell DJ, Ronksley PE, Hemmelgarn BR, et al. Association of enrolment in primary care networks with diabetes care and outcomes among First Nations and low-income Albertans. Open Med 2012;6:e155–65.
- Bhattacharyya OK, Rasooly IR, Naqshbandi M, et al. Challenges to the provision of diabetes care in first nations communities: Results froma national survey of healthcare providers in Canada. BMC Health Serv Res 2011;11:283.
- Rice K, Te Hiwi B, Zwarenstein M, et al. Best practices for the prevention and management of diabetes and obesity-related chronic disease among indigenous peoples in Canada: A review. Can J Diabetes 2016;40:216–25.
- Kakekagumick KE, Naqshbandi Hayward M, Harris SB, et al. Sandy Lake health and diabetes project: A community-based intervention targeting type 2 diabetes and its risk factors in a first nations community. Front Endocrinol (Lausanne) 2013;4:170.
- Perry RC, Shankar RR, Fineberg N, et al. HbA1c measurement improves the detection of type 2 diabetes in high-risk individuals with nondiagnostic levels of fasting plasma glucose: The Early Diabetes Intervention Program (EDIP). Diabetes Care 2001;24:465–71.
- Jin AJ, Martin D, Maberley D, et al. Evaluation of a mobile diabetes care telemedicine clinic serving Aboriginal communities in Northern British Columbia, Canada. Int J Circumpolar Health 2004;63(Suppl. 2):124–8.
- Panagiotopoulos C, Rozmus J, Gagnon RE, et al. Diabetes screening of children in a remote First Nations community on the west coast of Canada: Challenges and solutions. Rural Remote Health 2007;7:771.
- Vassalotti JA, Li S, McCullough PA, et al. Kidney early evaluation program: A community-based screening approach to address disparities in chronic kidney disease. Semin Nephrol 2010;30:66–73.
- Oster RT, Shade S, Strong D, et al. Improvements in indicators of diabetesrelated health status among first nations individuals enrolled in a communitydriven diabetes complications mobile screening program in Alberta, Canada. Can J Public Health 2010;101:410–14.
- Marley JV, Oh MS, Hadgraft N, et al. Cross-sectional comparison of point-ofcare with laboratory HbA1c in detecting diabetes in real-world remote Aboriginal settings. BMJ Open 2015;5:e006277.
- Shephard M, O’Brien C, Burgoyne A, et al. Review of the cultural safety of a national Indigenous point-of-care testing program for diabetes management. Aust J Prim Health 2016;22:368–74.
- Rudnisky CJ, Wong BK, Virani H, et al. Risk factors for progression of diabetic retinopathy in Alberta First Nations communities. Can J Ophthalmol 2012;47:365–75.
- Tapp RJ, Svoboda J, Fredericks B, et al. Retinal photography screening programs to prevent vision loss from diabetic retinopathy in rural and urban Australia: A review. Ophthalmic Epidemiol 2015;22:52–9.
- Davis TM, Hunt K, Bruce DG, et al. Prevalence of depression and its associations with cardio-metabolic control in Aboriginal and Anglo-Celt patients with type 2 diabetes: The fremantle diabetes study phase II. Diabetes Res Clin Pract 2015;107:384–91.
- Metzger BE, Gabbe SG, Persson B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–82.
- Chamberlain C, McNamara B,Williams ED, et al. Diabetes in pregnancy among indigenous women in Australia, Canada, New Zealand and the United States. Diabetes Metab Res Rev 2013;29:241–56.
- Chamberlain C, Fredericks B, McLean A, et al. Associations with low rates of postpartum glucose screening after gestational diabetes among Indigenous and non-Indigenous Australian women. Aust N Z J Public Health 2015;39:69–76.
- Jones EJ, Peercy M, Woods JC, et al. Identifying postpartum intervention approaches to reduce cardiometabolic risk among American Indianwomen with prior gestational diabetes, Oklahoma, 2012–2013. Prev Chronic Dis 2015;12:E45.
- Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403.
- Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: An intent-totreat analysis of the DPP/DPPOS. Diabetes Care 2012;35:723–30.
- Health Canada. Aboriginal diabetes initiative program framework 2010 - 2015. Ottawa, ON: Minister of Health. 2011. https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fniah-spnia/alt_formats/pdf/pubs/diseases-maladies/diabete/2010-2015-frame-cadre/2010-2015-adi_frame-cadre_ida-eng.pdf. Report No.: H34-156/2011E Contract No.: 110146.
- Gaudreau S, Michaud C. Cultural factors related to the maintenance of health behaviours in Algonquin women with a history of gestational diabetes. Chronic Dis Inj Can 2012;32:140–8.
- Narayan KM, Hoskin M, Kozak D, et al. Randomized clinical trial of lifestyle interventions in Pima Indians: A pilot study. Diabet Med 1998;15:66–72.
- Dill EJ, Manson SM, Jiang L, et al. Psychosocial predictors of weight loss among American Indian and Alaska Native participants in a diabetes prevention translational project. J Diabetes Res 2016;2016:1546939.
- Satterfield D, DeBruyn L, Santos M, et al. Health promotion and diabetes prevention in American Indian and Alaska Native communities–traditional foods project, 2008–2014. MMWR Suppl 2016;65:4–10.
- Nazarea VD, Rhoades RE, Andrews-Swann JE. Seeds of resistance, seeds of hope: Place and agency in the conservation of biodiversity. Tucson: University of Arizona Press, 2013.
- Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;Cd001871.
- Eskicioglu P, Halas J, Senechal M, et al. Peer mentoring for type 2 diabetes prevention in first nations children. Pediatrics 2014;133:e1624–31.
- Macaulay AC, Ing A, Salsberg J, et al. Community-based participatory research: sharing results with the community. An example of knowledge translation from the Kahnawake Schools Diabetes Prevention Project. Progress in Community Health Partnerships: Research, Education, and Action 2007;1:143–52.
- National farm to school network. Chicago, Il: National Farm to School Network (NFSN); 2017 [updated 2017]. Available from: http://www.farmtoschool.org./.
- Ritenbaugh C, Teufel-Shone NI, Aickin MG, et al. A lifestyle intervention improves plasma insulin levels among Native American high school youth. Prev Med 2003;36:309–19.
- Young T, Martens PJ, Taback SP, et al. Type 2 diabetes mellitus in children: Prenatal and early infancy risk factors among native canadians. Arch Pediatr Adolesc Med 2002;156:651–5. http://dx.doi.org/10.1001/archpedi.156.7.651.
- Sina M, Hoy WE, Callaway L, et al. The associations of anthropometric measurements with subsequent gestational diabetes in Aboriginal women. Obes Res Clin Pract 2015;9:499–506.
- Sinclair KA, Makahi EK, Shea-Solatorio C, et al. Outcomes from a diabetes selfmanagement intervention for Native Hawaiians and Pacific People: Partners in care. Ann Behav Med 2013;45:24–32.
- Townsend CKM, Dillard A, Hosoda KK, et al. Community-based participatory research integrates behavioral and biological research to achieve health equity for native Hawaiians. Int J Environ Res Public Health 2015;13.
- Aspin C, Brown N, Jowsey T, et al. Strategic approaches to enhanced health service delivery for Aboriginal and Torres Strait Islander people with chronic illness: A qualitative study. BMC Health Serv Res 2012;12:143.
- Sherifali D, Shea N, Brooks S. Exploring the experiences of urban first nations people living with or caring for someone with type 2 diabetes. Can J Diabetes 2012;364:175–80.
- Jacklin KM, Henderson RI, Green ME, et al. Health care experiences of Indigenous people living with type 2 diabetes in Canada. CMAJ 2017;189:E106–12.
- Crowshoe LL, Henderson RI, Green ME, et al. Exploring Canadian physicians’ experiences with diabetes care for Indigenous patients. Can J Diabetes 2017;30803–6. pii: S1499-267116.
- Naqshbandi Hayward M, Kuzmina E, Dannenbaum D, et al. Room for improvement in diabetes care among First Nations in northern Quebec (Eeyou Istchee): Reasonable management of glucose but poor management of complications. Int J Circumpolar Health 2012;71:1–8.
- Schoen DE, Norman PE. Diabetic foot disease in Indigenous people. Diabetes Manag 2014;46:489–500. http://dx.doi.org/10.2217/dmt.14.43.
- Curtis J, Lipke S, Effland S, et al. Effectiveness and safety of medication adjustments by nurse case managers to control hyperglycemia. Diabetes Educ 2009;35:851–6.
- Pylypchuk G, Vincent L, Wentworth J, et al. Diabetes risk evaluation and microalbuminuria (DREAM) studies: Ten years of participatory research with a First Nation’s home and community model for type 2 diabetes care in Northern Saskatchewan. Int J Circumpolar Health 2008;67:190–202.
- McDermott RA, Schmidt B, Preece C, et al. Community health workers improve diabetes care in remote Australian Indigenous communities: Results of a pragmatic cluster randomized controlled trial. BMC Health Serv Res 2015;15:68.
- Beckham S, Bradley S,Washburn A, et al. Diabetes management: Utilizing community health workers in a Hawaiian/Samoan population. J Health Care Poor Underserved 2008;19:416–27.
- Hotu C, Bagg W, Collins J, et al. A community-based model of care improves blood pressure control and delays progression of proteinuria, left ventricular hypertrophy and diastolic dysfunction in Maori and Pacific patients with type 2 diabetes and chronic kidney disease: A randomized controlled trial. Nephrol Dial Transplant 2010;25:3260–6.
- Gibson OR, Segal L. Limited evidence to assess the impact of primary health care systemor service level attributes on health outcomes of Indigenous people with type 2 diabetes: A systematic review. BMC Health Serv Res 2015;15:154.
- McDermott RA, Schmidt BA, Sinha A, et al. Improving diabetes care in the primary healthcare setting: A randomised cluster trial in remote Indigenous communities. Med J Aust 2001;174:497–502.
- McDermott R, Tulip F, Schmidt B, et al. Sustaining better diabetes care in remote indigenous Australian communities. BMJ 2003;327:428–30.
- Bailie R, Si D, Dowden M, et al. Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Serv Res 2007;7:67.
- Segal L, Nguyen H, Schmidt B, et al. Economic evaluation of Indigenous health worker management of poorly controlled type 2 diabetes in north Queensland. Med J Aust 2016;204:1961e–9.
- Gibson-Helm ME, Teede HJ, Rumbold AR, et al. Continuous quality improvement and metabolic screening during pregnancy at primary health centres attended by Aboriginal and Torres Strait Islander women. Med J Aust 2015;203:369–70.
- Harch S, Reeve D, Reeve C. Management of type 2 diabetes—a community partnership approach. Aust Fam Physician 2012;41:73–6.
- Harris SB, Green ME, Brown JB, et al. Impact of a quality improvement program on primary healthcare in Canada: A mixed-method evaluation. Health Policy (New York) 2015;119:405–16.
- Kotecha J, Brown JB, Han H, et al. Influence of a quality improvement learning collaborative program on team functioning in primary healthcare. Fam Syst Health 2015;33:222–30.
- Paquette-Warren J, Roberts SE, Fournie M, et al. Improving chronic care through continuing education of interprofessional primary healthcare teams: A process evaluation. J Interprof Care 2014;28:232–8.
- Ibiebele I, CooryM, Smith GCS, et al. Gestational age specific stillbirth risk among Indigenous and non-Indigenous women in Queensland, Australia: A population based study. BMC Pregnancy Childbirth 2016;16:159.
- Educating for equity ~ a tri-nations initiative. NewZealand; 2013 [updated 2013]. Available from: http://www.educating4equity.net.
- Kleinman A. Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine, and psychiatry. Los Angeles: University of California Press, 1981.
- Kumari M, Head J, Marmot M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Arch Intern Med 2004;164:1873–80.
- Gorringe S, Ross J, Fforde C. “Will the real Aborigine please stand up” : strategies for breaking the stereotypes and changing the conversation. Australian Institute of Aboriginal and Torres Strait Islander Studies. 2010. Available from: https://aiatsis.gov.au/sites/default/files/products/discussion_paper/gorringe-ross-fforde-dp28-real-aborigines-stereotypes.pdf.
- Stewart M, Brown JB, Weston WW, et al. Patient-centred medicine: Transforming the clinical method. UK: Radcliffe Medical Press, 2003.
- Brascoupé S,Waters S. Cultural Safety. Exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. J Aborig Health 2009;52:http://www.naho.ca/jah/english/jah05_02/V5_I2_Cultural_01.pdf.
- Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014;103:126–33.
- Esmail A. The prejudices of good people. BMJ 2004;328:1448–9.
- Wear D, Zarconi J, Aultman JM, et al. Remembering Freddie Gray: Medical education for social justice. Acad Med 2017;92:312–17.
- Ekong G, Kavookjian J. Motivational interviewing and outcomes in adults with type 2 diabetes: A systematic review. Patient Educ Couns 2016;99:944–52.
- Kezelman C, Stavropoulos P. Adults Surviving Child Abuse (ASCA). “The last frontier” practice guidelines for treatment of complex trauma and trauma informed care and service delivery. Kirribilli. Australia: Australian Government Department of Health and Ageing., 2012 http://www.recoveryonpurpose.com/upload/ASCA_Practice%20Guidelines%20for%20the%20Treatment%20of%20Complex%20Trauma.pdf.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;67: e1000097.
*The Canadian Diabetes Association is the registered owner of the name Diabetes Canada. All content on guidelines.diabetes.ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications@diabetes.ca.


