Recall
The 5 Rs for All Patients with Diabetes
What does this mean?
Recall is the step to implement in practice so that you develop a system to remind your patients and caregivers of
- Timely review and reassessment of targets
- Risk of complications, and,
- The need to recall your patients for regular visits
Why should I bother?
Having a recall system to remind your patients about timely tests and appointments will help you and your patient reassess their diabetes, and make adjustments to their care plan if necessary. As well, a reminder system for clinicians to recall patients for tests and appointments is a strategy to improve the quality of diabetes care.
OK. You’ve sold me. Where do I start?
Tips to promote recall and regular follow-up:
#1 When you and every healthcare provider on the team see a patient, discuss and agree whether and when patient recall will happen. Try to standardize recall intervals for equality of access, and also provide a system for your patients to receive rapid access and advice.
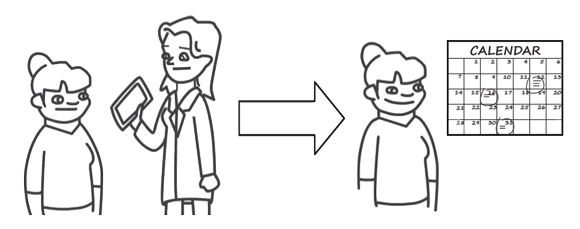
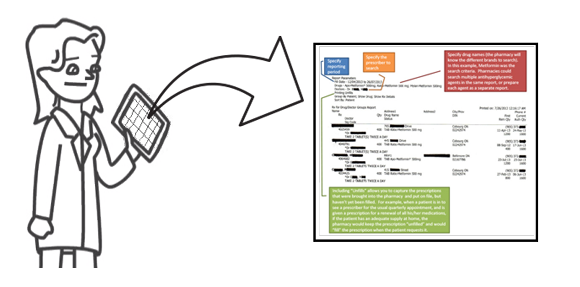
#2 If possible, give the patient their next appointment date and time prior to leaving the current appointment. If this is not possible, have a system in your practice to log the recall interval, and call to make the appointment later (i.e. EMR, computer spreadsheet, paper calendar or list, flag papers charts with diabetes sticker and review interval).
#3 To prepare for the next appointment, agree and communicate:
- 1) A plan of action with your patient between appointments
- 2) The purpose of the next appointment and review

It can be helpful for you to relay information with other healthcare providers on the team, and arrange tests (i.e. A1C, lipids or complication screening) prior to the next visit with your patient.
#4 Remind your patient of their upcoming appointment. Discuss and agree for how this will happen (i.e. telephone, text, appointment card) and when (i.e. one week before the appointment, one day before); this may help reduce no show rates. Electronic Medical Records can be programmed for alerts, and may link to diabetes registers.
Consider alternatives to office or clinic visits. This may be more acceptable to your patient, and efficient for the healthcare provider (e.g. phone, email, text, skype, secure diabetes website)
#5 Have plan for further recall, or discharge of ‘no shows’.
#6 Local practices will differ according to systems and resources. Among all members of the healthcare team, try to agree systems, processes and responsibilities for recall. Some areas might have a central diabetes register and a coordinator for booking appointments, rather than each individual healthcare provider being responsible for recall.
#7 Consider tracking performance indicators for recall, review intervals, % measurement of routine diabetes parameters, and % attainment of targets in your diabetes cohort.
A final important thought:
Healthcare providers should take responsibility for the recall process, and not leave the responsibility to the patient.
*The Canadian Diabetes Association is the registered owner of the name Diabetes Canada. All content on guidelines.diabetes.ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications@diabetes.ca.


