Screening for and Diagnosing Diabetes
Healthcare Provider Tool
Reset
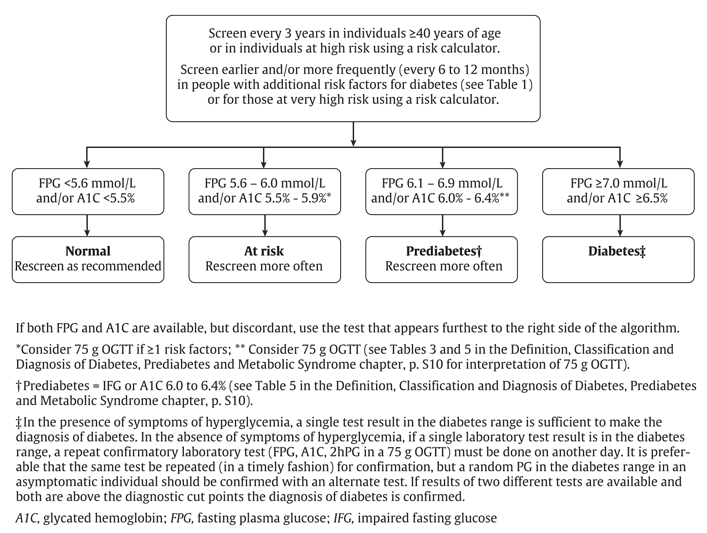
Measure Fasting Plasma Glucose (FPG) and/or A1C and enter test results:
| mmol/L | % |
Or
Measure 75g Oral Glucose Tolerance Test (OGTT) and enter test results:
| mmol/L | mmol/L |
Calculate Screening / Diagnosis Result
Calculate
This is only to be used as a decision support tool and is subject to these terms.
For more information, please see terms of use.
*The Canadian Diabetes Association is the registered owner of the name Diabetes Canada. All content on guidelines.diabetes.ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications@diabetes.ca.